Abstract
Background Chronic Graft vs. Host Disease (cGvHD) occurs in up to 60% of long-term survivors of allogeneic hematopoietic cell transplantation (alloHCT) and is associated with substantial morbidity and mortality. 1
Extracorporeal photopheresis (ECP) is an immunomodulatory therapy that has been used in the treatment of cGvHD, often in combination with steroids or other established immunosuppressants.
The purpose of this retrospective analysis of a registry database is to understand how ECP is being used within the real-world setting especially with introduction of newer immunosuppressants in particular ruxolitinib (RUX).
Methodology Data from the Center for International Blood and Marrow Transplant Research (CIBMTR) Registry was used. Inclusion criteria were patients in the United States who received an alloHCT during 2017 to 2019, were diagnosed with cGvHD within twelve months following alloHCT and received ECP for the treatment of cGvHD. Only data from centres who completed the Comprehensive Report Forms were included. For the analysis pre-specified end points were: Overall survival (OS) from date of first ECP±RUX treatment, and 'GvHD presence’ and 'GvHD still being treated with steroids or Immunosuppressants’ at last contact. Data was analysed by recipient, disease, transplant and post-transplant variables. OS survival was estimated by the Kaplan-Meier method.
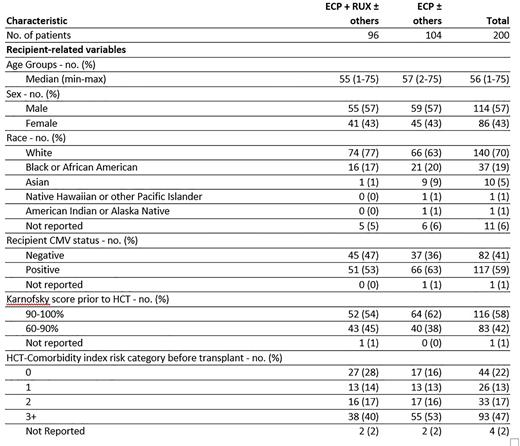
Results Of 2,435 patients who developed cGvHD within one year of alloHCT, 200 patients (8.2%) from 69 centres were eligible for the analysis. Median follow-up among all survivors was 35 months. The median age was 56 years (including 20 paediatric patients with median age of 11 years), 57% were males, and 70% White (Table). The majority of patients had prior aGvHD (79%), extensive cGVHD (95%) and were transplanted for a malignant disease (91%). Approximately 48% (n=96) of study patients had ECP in combination with ruxolitinib (ECP +RUX), either simultaneously, overlapping or sequential, with slightly younger age (55 vs 57 years) and higher percent of Caucasians (77% vs 63%) than ECP patients (n=104) without RUX (ECP-RUX)). The median time from cGVHD onset to ECP± RUX was 3 overall (range 0-43), 2 months for the ECP+RUX group and 3 months for ECP-RUX. For the ECP+RUX group, 52 (54%) patients had ECP treatment first and 38 (40%) had RUX treatment first (4 were same day and 2 unreported). Median time to switch or add in either ECP or RUX was 3 months and for 35% (33/96) of patients this occurred <1 month. The overall survival at year 1 and 2 following ECP+RUX or ECP-RUX treatment, were 77.4% vs 69.6% and 64.7% vs 52.9% (p=0.110), . Overall cGvHD presence at last contact was still high at 88% (n=176/200) and 53% (105) of patients were still taking steroids, while 63 patients (37%) stopped after ECP± RUX were initiated (10 patients stopped prior to initiation and for 12, the stop date was not reported) . In the ECP -RUX group 57% (19 /33) of patients stopped steroids < 6 months, compared to 30% (9/30) in ECP+RUX. Overall, 70% (139) were still taking an immunosuppressant agent (other than steroids), 74% and 65% in RUX+ECP and RUX-ECP, respectively.
Conclusion Results from this CIBMTR study using recent data show that ECP is used to primarily treat patients with extensive cGvHD. In nearly half the patients RUX was used in combination with ECP. Some differences were observed in characteristics and outcomes in the ECP group with and without RUX. Not all clinical outcomes and measures (in particular cGVHD response rates) were reported by centers or were only available at baseline, and data on all agents used to treat GvHD was not analysed. Despite these limitations, while cGvHD still persists in most patients, over a third of patients in our analyses were able to stop steroids .
References
1 Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol. Blood Marrow Transplant. 2003;9(4):215-233
Disclosures
Ingram:Mallinckrodt Pharmaceuticals: Current Employment. Shaw:OrcaBio: Consultancy; Mallinkrodt: Consultancy. Huang:Mallinckrodt Pharmaceuticals: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal